There are currently more than 3 million women living with breast cancer in the US, and it is the second leading cause of death among women. At some point during their lifetime, about 12% of women will be diagnosed with breast cancer.
While the death rate from breast cancer has declined overall, it remains the leading cause of cancer death among Hispanic women. Among African-American women, the incidence of breast cancer is lower than it is among white women, but the death rate is higher: by 2012, it was 42% higher—a difference that is expected to continue to grow. Even though many women are affected by breast cancer, many people may have questions about it. Read on to learn the facts.
What is breast cancer?
Breast cancer is caused by the uncontrolled growth of cells in the breast. These cells can form a mass called a tumor. Although breast cancers can start in different parts of the breast, most begin in the glands that produce milk (called lobules) or in the tubes (called ducts) that bring milk to the nipple.
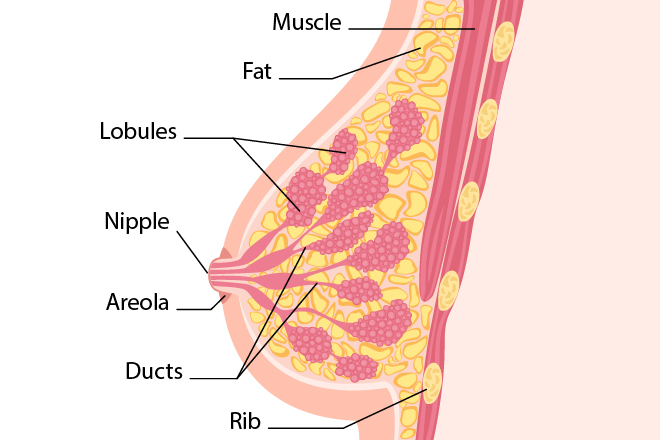
There are many different types of breast cancer. The most common types are carcinomas, which are named based on where they form and how far they have spread. The most common types of breast cancer are called ductal carcinoma in situ, invasive ductal carcinoma, and invasive lobular carcinoma. In situ is a noninvasive condition in which abnormal cells are found in the tissue where they began growing and have not invaded other tissue layers. Invasive means that the cancer has spread to other tissue in the breast.
There are two types of in situ cancers:
- Ductal carcinoma in situ (DCIS)—a non-invasive breast cancer, or breast cancer that has not yet spread from the ducts. The abnormal cells have not spread outside the duct to other tissues in the breast. In some cases, ductal carcinoma in situ may become invasive cancer and spread to other tissues. At this time, there is no way to know which lesions could become invasive. Also called DCIS and intraductal carcinoma.
- Lobular carcinoma in situ (LCIS)—a change in the breast that isn’t cancer. Cells that look like cancer are present within but not outside of the lobules in the breast.
There are many different kinds of invasive breast cancer, but the two most common are:
- Invasive ductal carcinoma—when the cancer cells spread from the ducts to other parts of the breast tissue. They can also spread (metastasize) to other parts of the body.
- Invasive lobular carcinoma—when the cancer cells spread from the lobules to other parts of the breast tissue that are nearby. They can also spread (metastasize) to other parts of the body.
Less common types of breast cancer include inflammatory breast cancer, Paget disease of the nipple, Phyllodes tumor, and angiosarcoma.
While most breast cancers occur in women, men can also develop it.
What causes breast cancer?
Most women who develop breast cancer have no clear risk factors for the disease and no family history of it. And having one or more risk factors does not mean that a woman will develop breast cancer. There are, however, certain risk factors that can increase a woman’s risk of developing breast cancer. These include:
- Age. Most breast cancers are found in women over age 50.
- Certain genetic mutations. Women who inherit mutations (changes) to certain genes (for example, BRCA1 and BRCA2) are at higher risk.
- Getting periods before age 12 or starting menopause after age 55. This causes a woman to be exposed to certain hormones for a longer period of time, which slightly increases her risk for breast cancer.
- Having dense breasts. This can make it harder to see tumors on a mammogram. Dense breasts have more connective tissue than fatty tissue.
- Family history. Having a first-degree relative (mother, sister, or daughter) or more than one family member on either the mother’s or father’s side who have had breast cancer increases a woman’s risk.
Research has shown that most breast cancers are caused by damage to genes that happens by chance after a person is born. Only 5% to 10% of breast cancers are inherited (when gene changes—called mutations—are passed from one generation of a family to the next).
Genetic mutations and breast cancer
Women who inherit genetic mutations to certain genes have a higher risk of developing breast cancer. Chief among these are genes called BRCA1 and BRCA2.
While all women have BRCA1 and BRCA2 genes, only about 1 in 500 women in the US has a genetic mutation in either gene. Not every woman with a mutation will get breast cancer, but it does put her at increased risk. Breast cancers linked to the BRCA1 or BRCA2 mutations are often found in younger women and more often in both breasts. Mutations in the BRCA1 and BRCA 2 genes also increase a woman’s risk of developing ovarian cancer.
In addition to mutations in the BRCA1 and BRCA2 genes, there are a number of other, less-common genetic mutations that can also increase a woman’s risk of developing breast cancer—though not as much as BRCA1 and BRCA2 mutations. These include ATM, TP53, CHEK2, PTEN, CDH1, STK11, and PALB2 genes.
Genetic testing can identify some women with inherited mutations in their BRCA1 and BRCA2 genes, as well as in certain other genes. This information can help them work with their healthcare providers to:
- Reduce their risk of developing breast cancer.
- Start screening for breast cancer earlier than a person who does not have the mutations.
- Take steps to look for and possibly prevent other cancers that are influenced by BRCA1 and BRAC2 genes.
- Learn if certain treatments are likely to be effective.
What are the signs and symptoms of breast cancer?
Most women diagnosed with breast cancer do not have any signs or symptoms of the disease. However, there are sometimes changes in the breast that a woman may notice. Any change should be brought to the attention of a healthcare provider. Changes to look out for include:
- A lump in the breast (the most common symptom of breast cancer).
- Swelling in the entire breast or in an area of it.
- Irritation on the skin or dimpling.
- Pain in the breast or nipple.
- Changes in the nipple or breast skin such as redness, thickening, or scaliness.
- A retracted (turned in) nipple or discharge from the nipple (other than breast milk).
How is breast cancer diagnosed?
A healthcare provider will usually order one or more diagnostic tests if:
- A woman finds a lump in her breast during a self-examination.
- A healthcare provider finds a lump or other breast changes during a physical examination.
- A screening mammogram shows a finding that requires more evaluation.
When should a woman have screening mammograms?
Finding breast cancer at an early stage means that a healthcare provider can begin treatment earlier in the course of the disease. Screening mammograms are an important diagnostic tool for early detection and have been shown to help reduce the number of deaths from breast cancer among women 40 to 74 years old.
In general:
- Women 40 to 49 years old may have a mammogram every 1 to 2 years.
- Women 50 to 75 should have a mammogram every 1 to 2 years depending on their risk factors.
- Women who have a mother or sister who had breast cancer at a younger age should consider having mammograms earlier than the age at which their youngest family member was diagnosed.
Women should talk with their healthcare provider about the screening mammogram schedule that’s best for them.
If breast cancer is suspected, the healthcare provider will perform one or more tests to make a diagnosis and/or to see if the cancer has spread to other parts of the body. The specific test depends on a number of factors, including:
- The type of cancer that is suspected.
- Signs and symptoms the woman may have.
- The woman’s age and medical history.
- Results from any earlier medical tests.
These tests may include imaging tests such as diagnostic mammograms (similar to screening mammograms but more images of the breast are taken), ultrasounds, and MRIs. These types of tests enable the healthcare provider to see the structure of a person’s breast.
Imaging tests are useful for suggesting if cancer is present, but only a biopsy can provide a definite diagnosis. During a biopsy, a healthcare provider removes small pieces of breast tissue using a needle or an incision and exams it under a microscope to see if cancer cells are present.
How is breast cancer treated?
Healthcare providers take a number of factors into account when deciding on a treatment plan for breast cancer. These include:
- If, how far, or how fast the cancer has spread.
- If the cancer cells have certain hormone receptors.
- The amount of a protein called HER2 in the cancer cells.
- A person’s health and personal preferences for treatment.
- Whether a woman has gone through menopause.
The most common treatments for breast cancer include:
- Surgery—Surgeons remove a portion of the breast containing the cancer or the entire breast.
- Chemotherapy—Medicines are given to shrink or destroy cancer cells.
- Hormonal therapy—Medicines are given to prevent cancer cells from getting the hormones they need to grow.
- Biological therapy—Medicines that work with the body’s own immune system to help it fight cancer cells.
- Radiation therapy—High-energy rays are used to kill cancer cells.
Most women with breast cancer typically receive more than one type of treatment.
Talk with your healthcare provider if you have any questions about breast cancer, screening, treatment, or steps you can take to reduce your risk. If you think you have any of the signs or symptoms of breast cancer, make an appointment to see your healthcare provider right away.
 Global Pharm Distribution, LLC
Global Pharm Distribution, LLC